Have you ever wondered what happens to the eggs and sperm inside the reproduction laboratory?
Once a couple visits a doctor or an embryologist, the case is submitted to the Fertility Specialists scientific team for research and examination. The team analyzes the scientific data and produces a treatment plan, in order to achieve the desired positive result. The role and experience of the embryologist are vital in this encounter, especially if the couple has had failed attempts in the past. The embryologist is the one responsible for interpreting the previous results.
The cycle begins with the stimulation of the ovaries in order to produce eggs.
The quality of the eggs and ultimately the fetus, depend on the careful stimulation of the ovaries, through individualized hormone therapy. After the administration of the Chorionic Genotropin (Hcg), the doctor collects the eggs from the follicles with a suction needle while using either local or general anesthesia.
The embryologist supervises the whole procedure, from the moment of ovulation until the transfer of the fetus back to the uterus.
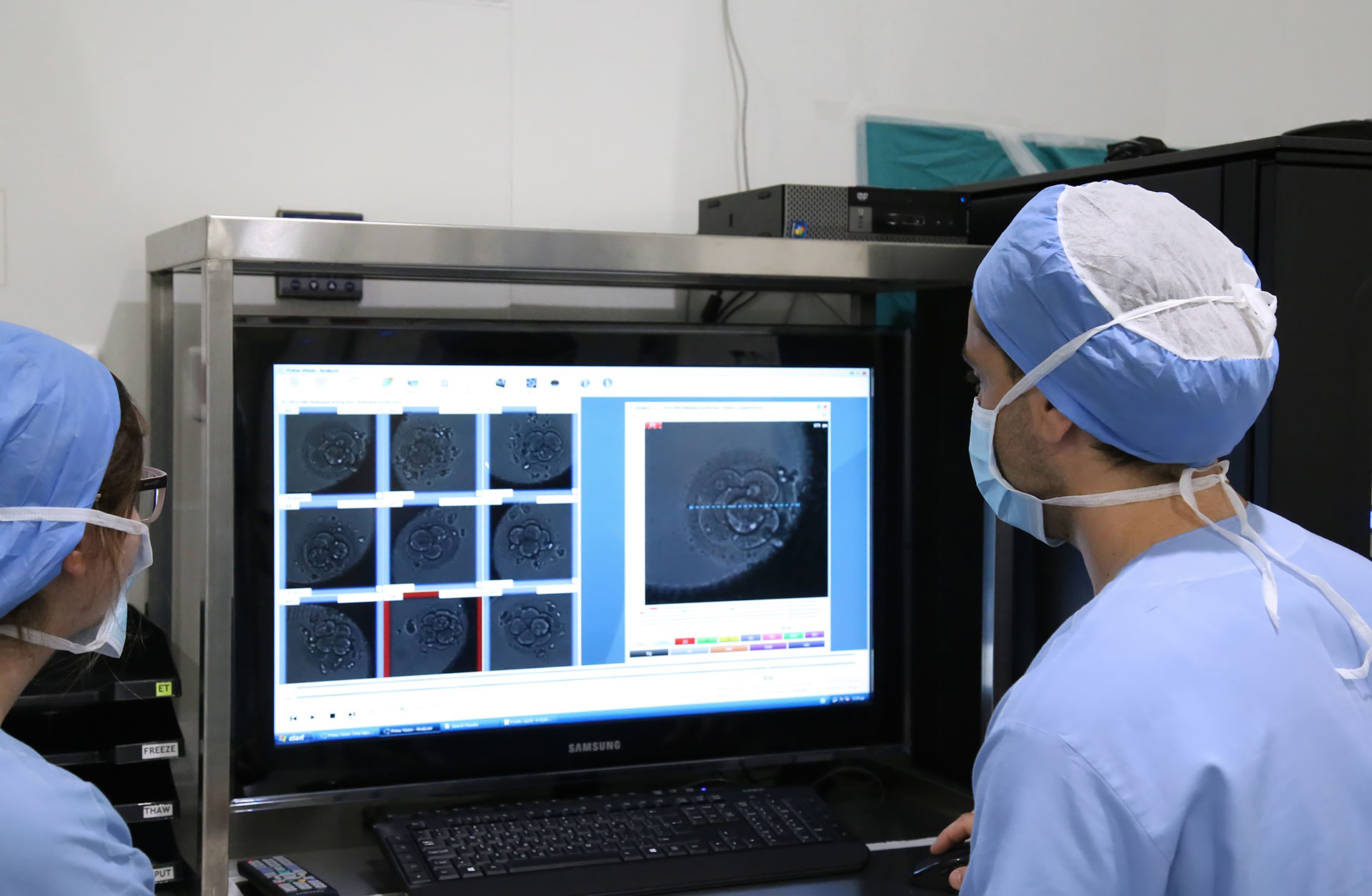
The embryologist’s workplace is the clinical laboratory which is configured to closely resemble the environment of the uterus. The light is dim and the temperature is high, just like in the human body. The fetus develops inside incubators that maintain the body temperature at 37°C. The embryologist makes sure that the fetus “grows” in conditions that are as similar as possible to the conditions of the uterus, in terms of normal pH and nutrients. This allows the fetus to develop with minimal environmental stress.
Every morning the embryologist carefully checks all the laboratory equipment before starting his work – Quality control.
Day 0
After the ovulation, the embryologist examines the follicular fluid through a stereoscope. The procedure is performed under controlled temperature and climate conditions. All the collected eggs are “washed” and placed directly on a dish through cultivation. They are then placed in the incubator. Simultaneously with the ovulation, semen is collected by ejaculation or Surgical Sperm Retrieval (SSR). Typically, the naturally ejaculated sperm is “washed” in order to remove the sperm plasma along with dead or slow-moving spermatozoa. At the end, only the active and swift sperm cells remain.
For people with more specific needs, there are other new techniques available. One of them is Magnetic Cell Separation (MACS). The next step for the embryologist is to fertilize the eggs with the sperm. The method used is the one that has been determined by the treatment plan from the beginning.
ClassicIn Vitro Fertilization (IVF)
This treatment is preferred in cases of blocked fallopian tubes, as long as there is no male infertility factor. The fast-moving sperm cells are collected in a tube and placed in cultivation plates along with their eggs and granule cells. They play an important role in sperm selection, as they move chemotactically. The plate is then placed back in the incubator so that, if everything goes well, the fertilization can begin.
Intracellular sperm injection (ICSI)
Until the early 90s, the only hope in cases of serious male infertility was the use of sperm from a donor. The ICSI technique became known in 1992 and is designed for those with severely reduced sperm quantity and motility. The embryologist tries to find an active, mobile sperm with good morphology, which must swim fast and in a straight line. When he discovers a suitable one, he uses the micro-fertilization pipette to stop its movement by tapping it on the tail. It is then taken and injected into the egg. The procedure is monitored by a special microscope, the use of which requires great skill and ability from the embryologist.
Day 1
After micro-fertilization is completed on Day 0, the eggs remain in the incubator for 18 hours.
It usually takes place overnight, until a re-examination is performed to determine if they have been successfully fertilized. The embryologist must follow a very strict schedule from when the micro-fertilization takes place until the fertilization check. This is a very important part of the procedure. More specifically, for 4 to 6 hours the embryologist has the ability to observe the number of pronuclei in the egg for fertilization. This indicates whether the egg has been fertilized normally or not. Research has shown that the orientation of the nucleoli within the “pre-nuclei” indicates an increased chance for the development of a normal fetus.
Day 2
Fetal developmental testing is performed daily.
The embryologist keeps a diagram where he notes down the various stages of fetal development in order to select the best ones to be transferred. These observations are necessary to distinguish the normally developing embryos from the rest. The goal is to increase the chances of implantation. Each clinic, however, usually has different criteria concerning the diagram it keeps.
Day 3 – 5
Between the 3rd and 5th day, the embryologist continues the daily examinations. While on day 3, the embryo consists of 6 to 8 cells.
By the 3rd day, the fertilized egg divides, using the energy accumulated during the follicular phase. On the 3rd day, the energy that further develops it into a blastocyst comes from the fetus itself and from this stage on, the fetus is considered energy independent. Day 3 is an extremely important transition point in human development. The embryos may stop growing on the 4th day, but if they continue to grow, their appearance changes and are henceforth called blastocysts.
A blastocyst is a cluster of 200 to 300 cells or more. Pregnancy rates tend to be higher if the woman participating in the IVF procedure undergoes blastocyst transfer, since the cells have already gone through a significant developmental stage. Nevertheless, many pregnancies succeed even if the transfer occurs on the 2nd or 3rd day. The successful transition from the fetus stage to the blastocyst stage depends on the equipment, skills and knowledge of the embryologist in regards to the IVF procedure.
Embryo transfer
An embryo transfer can take place on the 3rd and 5th day.
Choosing when the embryo transfer will take place is crucial and depends on many factors. The purpose, however, is always unique: to increase the chances of a healthy pregnancy. The lower the quality of the embryos, the sooner they should be transferred. As long as the choice is clear, the embryologist will monitor the fetus only for the necessary time required to guarantee secure embryo development for a successful IVF procedure. An early transfer of the fetus would ensure protection from the artificial environment.
On the other hand, in cases where there is a larger amount of good embryos, the transfer usually takes place at a later day (on the 5th day for example).
This allows the embryologist to benefit from the changes that occur naturally on the 3rd day
by separating the embryos that are least likely to be implanted. The embryos that are kept, are the ones with the highest chances of implantation. Depending on the case, either one or two good quality embryos are selected to be transferred by the embryologist to the uterus. If there are any more good quality embryos that have not been transferred, they are frozen and stored.
Preimplantation Genetic Screening (PGS)
Despite the embryologist’s regular checks, there are some fetuses that look normal and healthy but may actually have genetic anomalies that will lead to failed implantation or recurrent miscarriages. Preimplantation diagnosis involves testing the fetal chromosomes for common deformities, like in the case of an embryo with the wrong number of chromosomes (aneuploidy). In those cases, the embryologist removes one or two cells from the embryo on the 3rd day or an even greater number of cells from the trophectoderm of the embryo on the 5th day. He then examines them in order to secure the success of the IVF procedure.
Dimitris Papadopoulos, Clinical Embryologist, Rea Maternity Hospital.